Subscribe to Receive Updates
Join hundreds of business leaders and get our perspective on critical issues delivered to your inbox..

We all love a good checklist – until it gives us a false sense of security. For small medical practices, dental clinics, and behavioral health centers, HIPAA IT compliance checklists often serve as the primary tool for staying audit-ready. But here’s the uncomfortable truth: most checklists being used today are dangerously incomplete.
They focus on documentation, not detection. Policies, not practices. Many are repurposed from outdated templates or only touch on surface-level requirements. And while they might help you feel “covered,” they won’t protect your systems (or your patients) when real-world threats hit.
At thirtyone3 technology, we work with healthcare providers who believed they were secure, until they weren’t. Breaches, fines, and patient data exposures rarely happen because someone forgot to check a box. They happen because what’s not on the checklist is often what matters most.
Take for example a behavioral health clinic that checked “encryption” off their list, only to discover months later that their vendor only encrypted data in transit, not at rest. Or an office with neatly organized risk assessments… with zero follow-up actions taken. These aren’t rare cases, they’re common oversights we encounter regularly.
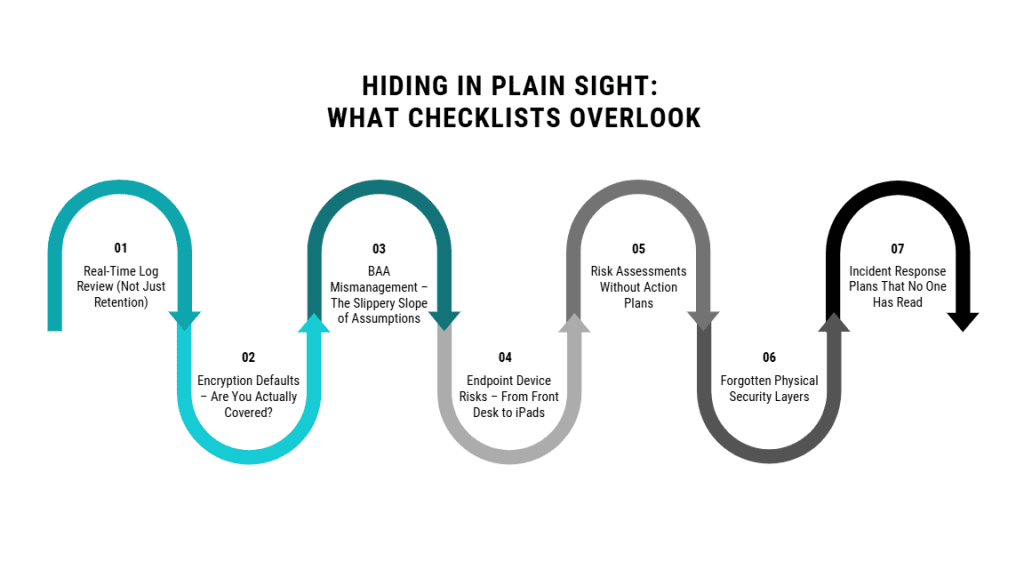
In this Insight, we’ll explore seven critical areas missing from most HIPAA IT compliance checklists, and why these gaps could cost your practice more than just an OCR fine. We’ll draw from real-world missteps, federal expectations, and proven solutions used by forward-thinking clinics across Arizona. Because a checklist can guide you, but it won’t save you.
Ask most clinics about their audit logs, and they’ll tell you everything’s covered; they retain logs for the required six years. But retention isn’t the same as real-time visibility. In fact, this is one of the most dangerous blind spots in the average HIPAA IT compliance checklist.
The HIPAA Security Rule requires covered entities to implement audit controls that record and examine activity in information systems. But it doesn’t stop there. According to the HIPAA Journal, the expectation extends to proactively reviewing these logs for signs of unauthorized access, system misuse, or potential breaches.
Unfortunately, many small clinics and outpatient centers lack the tools or personnel to review logs consistently (if at all). This leaves them vulnerable to undetected threats that quietly escalate: a disgruntled employee accessing patient files, a misconfigured user role, or a compromised login pulling data after hours.
We’ve worked with practices in Phoenix who had full audit trails… they just weren’t looking at them. And in several cases, the damage was done by the time anyone noticed.
Logs aren’t useful if no one’s watching. A managed detection and response (MDR) solution, or even basic alerting tied to anomalous access patterns, can dramatically reduce your response time. And in the eyes of an OCR auditor, not reviewing your logs regularly is considered a risk, not a gap in paperwork.
Encryption is one of those checklist items that gets a quick checkmark, “Yes, our system is encrypted.” But when we dig deeper, the story often changes.
Many EHR platforms and practice management systems offer encryption in transit, meaning data is protected while it’s being sent. However, that doesn’t mean the data is protected when it’s stored (at rest) and HIPAA requires both.
Relying on a vendor’s generic security statement or assuming all encryption is equal is a recipe for noncompliance. We’ve encountered clinics storing backups unencrypted on local Network Attached Storage (NAS) drives, or relying on unverified settings in cloud storage platforms. If that data is accessed or stolen, the absence of full encryption could lead to both breach notification requirements and financial penalties.
Covered entities must implement a mechanism to encrypt and decrypt electronic protected health information. Importantly, this is not a passive checkbox, it’s an active responsibility to ensure encryption is configured properly across all systems, backups, and devices.
The takeaway? Don’t assume “encrypted” means compliant. Verify, document, and test your encryption settings across the entire data lifecycle.
Most clinics understand the need for Business Associate Agreements (BAAs), but very few manage them well.
A typical HIPAA checklist asks, “Do you have BAAs in place with all vendors who handle PHI?” That’s a good start. But what it misses is whether those agreements are current, enforceable, and sufficient to protect your clinic if something goes wrong.
It’s not uncommon for smaller practices to:
This is dangerous. If your cloud-based billing platform, IT provider, or document storage service suffers a breach and you don’t have a valid BAA, your clinic can be held directly liable under HIPAA.
If you haven’t reviewed your BAAs in the last 12 months, that’s a red flag. Each vendor relationship should be documented, legally bound, and periodically reevaluated to reflect any changes in services or risk.
Because if OCR knocks on your door, “we thought they had it covered” won’t hold up.
Walk through a typical outpatient clinic and you’ll see it: front-desk desktops with sticky notes, unsecured laptops at nurse stations, personal tablets used during patient intake. These endpoint devices are the soft underbelly of most HIPAA environments, and they’re often completely overlooked in compliance checklists.
While policies may mention device security in broad strokes, they rarely go far enough. Without centralized management, devices can go unpatched, unencrypted, or left logged in. A lost tablet, a stolen laptop, or even a reused password on a personal phone can lead to a reportable breach.
This isn’t hypothetical. We’ve seen Phoenix-based practices penalized after an employee’s unprotected laptop containing patient data was stolen from their car. The incident wasn’t the theft, it was the lack of endpoint controls.
In fact, some of the most costly HIPAA mistakes we’ve seen come from overlooked device management in behavioral health clinics, where high patient turnover and mobile workflows create even more risk. If you’re unsure how your front-desk terminals, iPads, or personal staff devices are secured, review our breakdown of common IT security mistakes outpatient behavioral health clinics can’t afford to make.
If your HIPAA checklist doesn’t ask how devices are monitored, secured, and recovered, it’s missing one of your most exposed vectors.
Many clinics can proudly point to a completed Security Risk Assessment (SRA), often conducted by a third-party vendor or filled out using an online template. But having an SRA on file doesn’t equal compliance. What matters most is what you do with it.
HIPAA requires not just an assessment of risks and vulnerabilities, but also a plan to mitigate them. This includes documenting which risks were identified, assigning responsibility, setting deadlines, and following through. Too often, however, SRAs become static documents – read once, filed away, and forgotten.
This kind of gap is exactly what regulators look for. During audits, investigators look for more than just an assessment. They expect clear evidence that identified vulnerabilities have been addressed through measurable, timely remediation efforts. As noted by compliance experts, lacking follow-up on risk findings is one of the top reasons practices fail OCR audits.
We’ve worked with clinics that had all the right findings listed (unsecured remote access, outdated firmware, weak password policies), but no documented response. In an audit, that’s a red flag.
If your HIPAA IT compliance checklist stops at “conduct annual risk assessment,” it’s only half the story. The follow-through is where the real protection begins.
In the digital age, it’s easy to forget that HIPAA is just as concerned with physical access as it is with firewalls and encryption. Yet, in most small practices, physical security is one of the least enforced elements of compliance, and one of the most commonly overlooked on checklists.
We’ve walked into clinics where server closets are propped open with a chair, or where backup drives sit unsecured in desk drawers. Cleaning crews, temp staff, and vendors often have untracked access to areas storing protected health information (PHI), creating silent opportunities for theft or tampering.
HIPAA requires covered entities to “implement physical safeguards” to limit physical access to electronic information systems and the facilities in which they are housed. That includes everything from badge-controlled access, surveillance, and visitor logs to lockable storage for portable devices and backups.
OCR has issued penalties for breaches involving stolen computers from unlocked rooms and patient files left exposed in multi-use office spaces. These aren’t sophisticated hacks, they’re simple lapses in everyday physical control.
If your compliance checklist doesn’t ask who has access to what, when, and how it’s logged, your clinic could be vulnerable in the most low-tech (but high-risk) way possible.
Every HIPAA compliance binder has one: an Incident Response Plan (IRP) written months or even years ago, tucked between policy templates and onboarding paperwork. But when a real incident happens – ransomware, unauthorized access, a lost laptop – no one knows what to do, because no one’s ever read the plan.
HIPAA requires that covered entities not only have an incident response policy but also that they can demonstrate how it’s implemented. This means your team must know the process, roles must be clearly assigned, and the plan must be tested regularly. Yet, this is rarely included, or properly detailed, on standard HIPAA IT compliance checklists.
We’ve seen practices freeze during a breach event, unsure who to notify, what to shut down, or how to document the timeline. The delay alone can escalate the impact and the consequences.
The best IRPs are living documents. They are updated annually, role-played in tabletop exercises, and tailored to real workflows. If your staff wouldn’t know how to respond to a ransomware email or a data exfiltration alert, the plan isn’t doing its job.
A checklist item labeled “incident response plan: yes/no” doesn’t reflect whether your clinic is truly ready. The question should be: Has it been tested, trained, and updated?
It’s tempting to see HIPAA compliance as a paperwork exercise until something goes wrong.
The Office for Civil Rights (OCR) isn’t just auditing for missing documentation anymore. They’re evaluating whether your clinic’s safeguards actually function in practice. This means the superficial checklist that once seemed sufficient could now expose you to six-figure penalties, breach investigations, or even temporary suspension of operations.
And that’s just the regulatory risk.
When a breach occurs, the damage spreads far beyond fines. Patient trust erodes. Referral partners take notice. Leadership shifts focus from growth to damage control. For small and midsize clinics, this kind of fallout can take years to recover from, if recovery is even possible.
We’ve worked with Phoenix-area practices that discovered these gaps too late; BAAs signed but not updated, logs retained but never reviewed, risk assessments with no action taken. In every case, the cost of inaction was higher than the cost of preparation.
These aren’t obscure technical failures. They’re the basics, and missed simply because no one thought to look beyond the checklist.
And small clinics are especially vulnerable. Without dedicated compliance officers or in-house IT teams, it’s easy to assume that vendors or policies have things “handled.” But OCR holds the clinic (not the vendor) accountable.
Ignoring the gaps doesn’t make them harmless. It just makes them hidden.
Proactive clinics don’t stop at compliance, they focus on resilience.
The practices we see thriving under HIPAA scrutiny and operational demands take a fundamentally different approach. Instead of relying solely on templated checklists or once-a-year risk reviews, they treat security and compliance as living systems; monitored, tested, and improved over time.
What does that look like in real terms?
This level of maturity doesn’t come from internal effort alone. It comes from partnering with MSPs that understand HIPAA, offer 24/7 monitoring, and provide both strategic guidance and tactical execution.
At thirtyone3 technology, we work with clinics across Arizona to build compliance strategies that go beyond templates. From real-time threat detection to BAA lifecycle management, our approach is designed to help small practices stay audit-ready without sacrificing clinical uptime.
Because checklists are helpful, but real security is measurable, maintained, and always moving.
Compliance checklists serve a purpose, but they were never meant to be your entire HIPAA strategy.
They can’t tell you if your devices are encrypted correctly. They won’t alert you to a breach. They don’t know whether your staff has ever run a response drill or if your last risk assessment actually led to change.
The truth is, what’s missing from most HIPAA IT compliance checklists are the things that matter most when the real world intrudes. Ransomware doesn’t care if you filed your BAA. OCR doesn’t give credit for policies no one follows. And your patients won’t forgive a data breach because you checked the right boxes.
At thirtyone3 technology, we help Phoenix-area clinics uncover and address these gaps, before they become liabilities. Whether you need real-time log monitoring, BAA lifecycle support, or just a fresh look at your current HIPAA posture, we’re here to help.
Let’s turn your checklist into something stronger: a system that actually protects what matters.
Join hundreds of business leaders and get our perspective on critical issues delivered to your inbox..